History taking is of paramount significance when it comes to diagnostic procedures being carried out at a hospital. A good history and examination requires sound knowledge of medicine, understanding of clinical conditions (and their manifestations) and communication skills. It is the first and the foremost part of the general diagnostic procedure and the whole foundation of medical diagnosis and management relies on it.
For those medical students who are about to start their clinical rotations (during the 3rd year of medical school as it happens here in Pakistan), it is very important for them to familiarize themselves to the hospital environment and learn the protocols in order to better communicate with the patients and have better learning outcomes.
In this post we will try to cover the important aspects of medical diagnostics and things that make-up a good history. But before that we go on in details of good history taking, making differentials and the art of patient management — lets take a look what the experts have to say! 🙂
Expert Tips for History Taking, Differentials and Patient Management
In order to make this article more accurate, informative and helpful — we requested some of the experts to share with us their valuable experience regarding history taking, differentials and patient management and here’s what they said:
DR. SAAD SHAFQAT (Professor of Neurology, Aga Khan University Hospital, Karachi)

PHOTO: Dr. Saad Shafqat
History taking:
The key is to be attentive and unbiased; gather data with an open mind; then shape it into diagnostic coherence using your clinical experience and your knowledge of pathophysiology. The greater your experience and knowledge, the better you will become at this foundational skill that represents the first step of the patient-physician encounter.
Differentials:
A common pitfall in diagnostic reasoning to list a large number of possible diagnoses. There is an expectation that the longer your differential, the “smarter” you are. Differentials are actually a list of what the diagnosis is not. To properly serve your patient, diagnosis requires finding the single best possible explanation. One of my professors used to say,
“Do you want the differential or do you want the answer?”
That is an important lesson to absorb.
Patient management:
Making the patient better should always be foremost in your thoughts. Read widely and stay up-to-date. Be well-versed with the latest guidelines in your specialty. Be knowledgeable about the side-effects of your treatments. Know when a treatment recommendation is evidence-based versus when it is a matter of anecdotal experience and judgment. Be mindful of expense but do not shy away from evidence-based treatment simply because of cost. Evaluate the benefit of treatment in terms of functionality and quality of life. And never forget the starting principle of medical service, primum non nocere (is a Latin phrase that means “first, do no harm.”).
DR. SYED AINAN ARSHAD (Instructor in Department of Internal Medicine at Aga Khan University Hospital, Karachi)

PHOTO: Dr. Syed Ainan Arshad
History Taking:
Traditionally it was said that history taking is an art. Still this principle is on. The good history taking would be fruitful for the whole management. You should have core knowledge of common symptoms and diseases especially prevalent in your setup. Always first think of common medical conditions prevalent in that area. And always listen to the patient and focus on his main complaint. As it is always a good clue. In short good history taking makes correct diagnosis and treatment easy.
Differentials:
Always ask and evaluate for differentials while taking history to include or exclude certain diseases. Differentials always give you a broader way of thinking and proper diagnosis. In exams differentials are always asked. And in MCQs these differentials appear in one best MCQs and those who have habit of excluding in history can appear well in MCQs exams as well.
Patient Management:
I think everything is interrelated and sequential. It depends on good history taking, examination findings, excluding differentials will make proper diagnosis and then management of that case. And again we should know the treatment, diagnostic modalities and common complications and side effects of treatments so that we can explain these things in advance. Remember everything should be fully explained to the patient. And of course your critical thinking and knowledge should always be evidence based.
DR. SHEEMA BALOCH (MBBS, PGR1 at Fauji Foundation Hospital, Islamabad)
History taking is a true form of performing arts. The command of one’s own self is what sets the pace. Undoubtedly the doctor is not there to make friends but the mannerism and accurate communication while taking history is what allows the patient to speak vividly to the doctor. Specially in emergency situations when a patient is not stable and the communication has to be with the attendant. The keenness of a doctor as a listener is definitely re-assuring to both the patient and the attendant.
Remember! No one nails the perfect diagnostic history in the first attempt, the more effort you put the closer you are to being perfect. Listen and co-relate, differentials are the key, even if things are evident, never close doors neither leave anything to assumption of being unimportant.
P.S. Develop skills to create correct associations by only listening and looking at the patient.
DR. SHAIKH ZARAK KHAN MANDOKHAIL (MBBS, USMLE Step 2 CK)
PHOTO: Dr. Shaikh Zarak Khan Mandokhail
A good doctor-patient relationship starts with an introduction (which involves greeting and a warm handshake) and patient-oriented working mechanism. Try not scurrying to make a quick judgment. Let the patient speak by asking open-ended questions. Hearing the patient’s account of his illness comes at the heart of building trust and patient satisfaction. And always try being a good listener, show respect to the patient, empathize and try managing the psychology of the patient because he is already going through much.
Introduction to History Taking
History taking, in short, is an interview with the patient which is aimed to have a thorough understanding of the patient’s illness and reasons that have caused him to visit the hospital. It can be defined as:
to know about the patient’s illness as he knows.
A history (Hx.) well-taken leads to the establishment of correct diagnosis and also helps to order relevant and targeted lab investigations which make treatment cost-effective for the patients.
And a widely quoted aphorism states:
Listen to your patient; they’re telling you the diagnosis.
History taking is an examination skill necessary for you as a doctor/student regardless of your area of practice and specialization. It’s something you will always be doing throughout your career while handling diagnostics.
General Guidelines
Before going into further details of history taking, lets take a look at some of the important guidelines that you need to keep in mind:
- Your dressing and overall appearance should be professional and in compliance to medical code of ethics.
- Your approach to the patient should be sympathetic, gentle, friendly and confident and not arrogant, humiliating and belittling. You must not exploit the power of your position and evoke a feeling of superiority in the patient’s mind. You must practice empathy and humility.
- You should start by introducing yourself with the patient.
- You should communicate with the patient in a language he understands well and is comfortable with.
- A female patient shall be given consultation either by a female medical or dental practitioner or shall be examined in the presence of a female attendant by a male doctor. [source: PMDC Code of ethics]
- A good listener makes a good doctor and listening comes at the heart of good history taking. So, listen to the patient attentively before making follow-up questions.
- Behave professionally especially when you’re working with the patient with a group of your colleagues. Show respect and courtesy to the patient and ask all your group mates / colleagues to be serious and not to make fun or laugh while inside hospital premises.
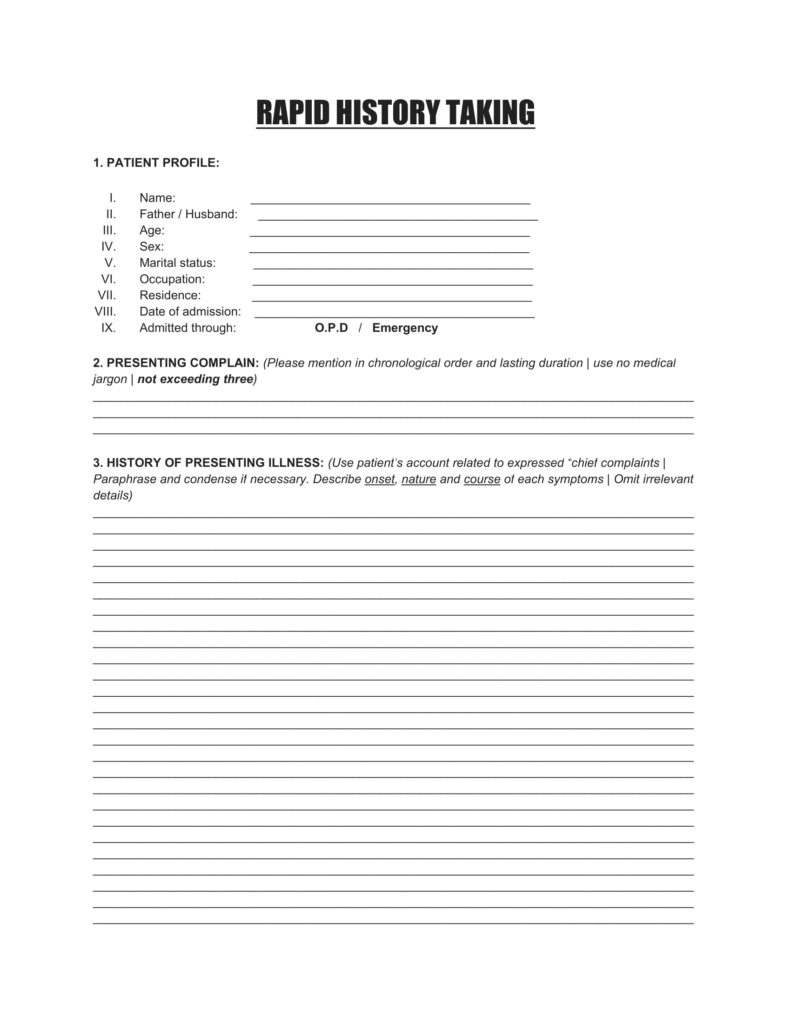
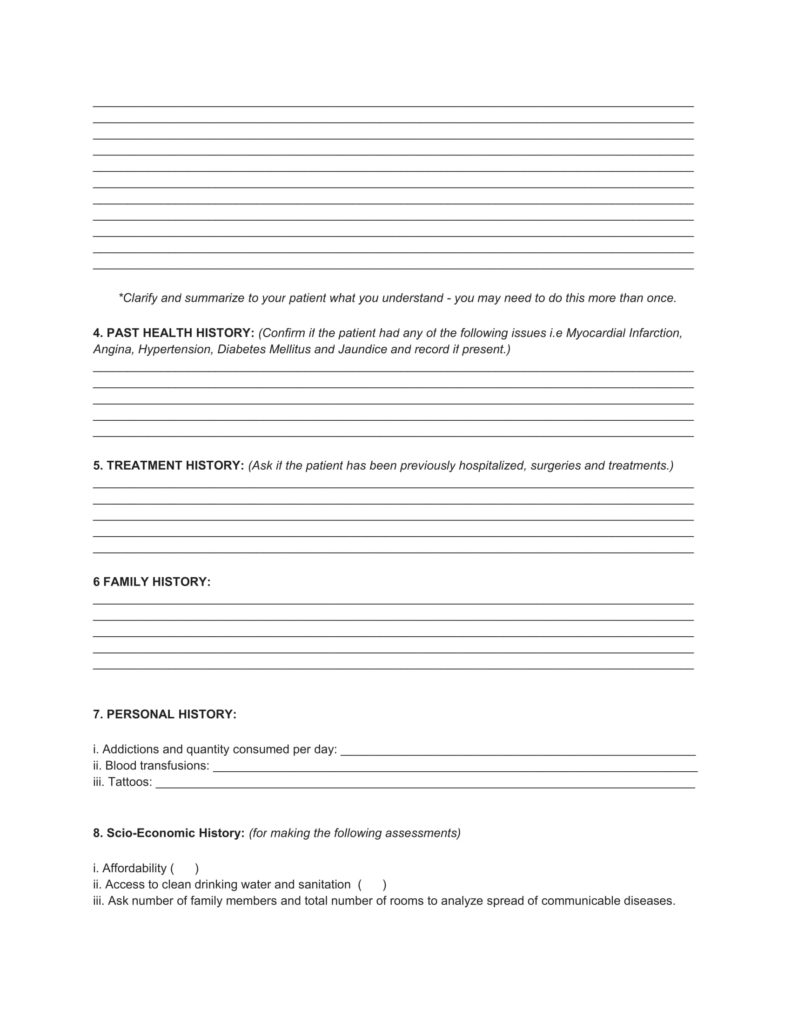
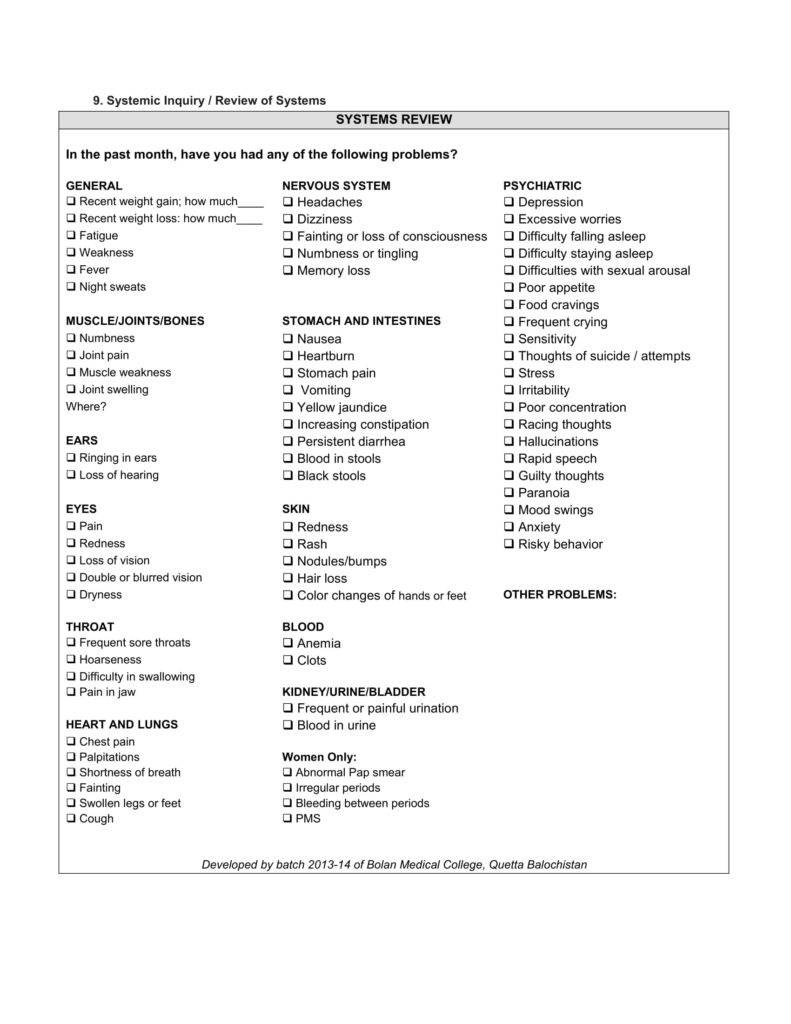
RAPID HISTORY TAKING FORM
Our colleagues, with a joint collaborative effort developed a rapid history taking form which we think will greatly help medical students who are about to start their clinical rotations.
Here’s what it looks like:
CLICK HERE TO DOWNLOAD RAPID HISTORY TAKING FORM
COMPONENTS OF HISTORY TAKING
A medical history consists of 10 components and it should be recorded in the same pattern as seen below:
- Introduction and consent
Once you find the patient you are to work with, start by making a good handshake (but only if the patient is not of the opposite gender) while having a polite smile on your face and make eye contact, introduce yourself and gain consent fort taking their history.
Here’s an example of how you can introduce yourself:
Greetings (Asalam Alekum)! My name is XYZ, I am a 3rd Year medical student
and I am here to examine you / to take your history. Should you have any problems during the procedure, please let me know.
2. Patient Profile (PP)
The patient profile consists of important details regarding the patient that are to be recorded for reference purpose and in some conditions, the P.P could also be useful in early diagnosis of an acquired disease as in case of an endemic or an epidemic by the knowledge of patient’s residency. Or details like occupation can be helpful in diagnosing occupational diseases such as Chronic obstructive pulmonary disease (COPD) in coal miners.
The patient profile consists of:
- Name of the patient
- Father / husband name
- Age
- Sex
- Marital Status
- Occupation
- Residence
- Date of admission
- Admission through: OPD / Emergency
3. Presenting Complaints (PC)
To put it in simple words, the presenting complaints are the reasons which have brought the patient to the hospital and this happens when the patient has reached the limits of tolerance. The presenting complaints should be carefully noted down in chronological order (mentioning the symptoms that developed first at the top followed by rest in sequence of occurrence). In addition, mention the duration of each complaint in front of it as seen in the below example:
- Pain in the right hypocondral region: 6 days
- Vomiting: 4 days
- Loose motions: 3 days
The presenting complaints should not exceed three.
4. History of Presenting Illness (HOPI)
The history of presenting illness or HOPI is considered to be one of the most important parts of the history taking because it helps in establishing a proper diagnosis and management of the patient’s illness. In this segment, you have to describe and investigate (by asking questions) the presenting complaints in detail one by one in sequence of their development.
Try collecting as much information regarding each presenting complaint in detail as you can. Take for example “pain in the right hypochondral region” from the aforementioned P.C, you can further investigate PAIN by asking the following questions:
Mnemonic: SOCRATES
- Site
- Onset
- Radiation
- Association
- Time course
- Exacerbating (aggravating) and relieving factors
- Severity of pain
DON’Ts: Use patient’s own words and do not use medical jargon i.e write breathlessness during night instead of paroxysmal nocturnal dyspnea.
**PRO TIP: Ask highly targeted and relevant questions regarding each presenting complaint and do not get yourself LOST. And always ask specific questions to the patient and do not let the patient deviate from the main complaint. Keep the steering of your history towards a diagnosis else you will end-up getting lost. Never ask questions like, “Do you have pain in the entire body?”, patients always tend to respond affirmative to such questions.
5. Systemic Inquiry
In this segment you have to collect small amounts data regarding the other systems of the body that are not covered in the history of presenting illness (HOPI). Suppose you have a patient with cardiovascular disorders so when you start the systemic inquiry, you can skip the CVS and focus on other systems by asking their cardinal symptoms.
The main systems of the body that need to be explored on systemic inquiry of history taking are:
- General (involves appetite, weight gain / loss, sleep pattern, energy)
- Cardiovascular System
- Respiratory System
- Alimentary System
- Urinary System
- Nervous System
- Skin
- Musculoskeletal System
IMPORTANCE: The systemic inquiry completes the history taking process as it helps exploring areas which have not been given attention earlier in the HOPI. Sometimes the patient tends to state symptoms which he thinks are important thus ignoring other symptoms by considering them unimportant. That is where systemic inquiry comes into play. It helps us focusing on illnesses and their symptoms which could have been missed.
6. Past Health History
- Ask if the patient has been previously hospitalized or not. If yes, investigate why and what kind of treatment did he receive.
- Ask if the patient has undergone any surgical procedures.
- Congenital anomalies
7. Menstrual History
8. Treatment History
Here you have to find out if the patient is taking any medications, if yes, then find out dosage and how many times he is taking them e.g once a day, twice a day etc.
IMPORTANT: Ask if the patient has allergies particularly to drugs and also record if the patient has any previous drug reactions.
9. Family History
Gather information about the patient’s parents, siblings and children and find out if any of them is suffering from a similar illness or a chronic illness i.e diabetes mellitus, hypertension, tuberculosis and ischemic heart disease. And if any of them is dead, find out why?
10. Personal History
- Ask about patients bowl movements, sleep habits and if he has any addictions i.e snuff, smoking and alcohol
- Tattoos
- Blood transfusions
11. Socio-Economic History
It is to assess the financial conditions of the patient which helps the doctor to device a suitable treatment plan keeping in view affordability.
You may write it as, “The patient HAS / DOES NOT HAVE access to clean drinking water and proper sanitation”. This statement gives enough idea to the reader.
Ask number of family members and total number of rooms to analyze possible spread of communicable disease.
When you think that you have completed your history taking and you have all of the information you require, you must thank the patient for their time and cooperation and say that one of the doctors / postgraduate medical residents (PGR) looking after them will be coming to see them soon.
Books Recommended for Learning History Taking & Clinical Examination
Here are two of the highly read and recommended books for you to learn and master the art of history taking and clinical examination:
We hope you found this post useful in terms of learning! 🙂
GOOD LUCK!


![Community Medicine Prof. Viva Questions [4th Year MBBS]](https://www.medicosrepublic.com/wp-content/uploads/2018/06/Community-Medicine-Prof-Viva-Questions-218x150.jpg)
![Special Pathology Viva Questions [4th Year MBBS] Special Pathology Viva Questions](https://www.medicosrepublic.com/wp-content/uploads/2018/06/Special-Pathology-Viva-Questions-218x150.jpg)





![Gerstmann Syndrome Features Mnemonic [Easy-to-remember] Gerstmann Syndrome Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Gerstmann-Syndrome-Features-Mnemonic-150x150.jpg)
![Cerebellar Signs Mnemonic [Easy to remember] Cerebellar Signs Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Cerebellar-Signs-Mnemonic-150x150.jpg)
![Seizure Features Mnemonic [Easy-to-remember] Seizure Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Seizure-Features-Mnemonic-1-150x150.jpg)
![Recognizing end-of-life Mnemonic [Easy to remember]](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Recognizing-end-of-life-Mnemonic-150x150.jpg)

![Multi-System Atrophy Mnemonic [Easy-to-remember] Multi-System Atrophy Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Multi-System-Atrophy-Mnemonic-150x150.jpg)

![How to Remember Southern, Northern, and Western Blot Tests [Mnemonic] How to Remember Southern, Northern, and Western Blot Tests](https://www.medicosrepublic.com/wp-content/uploads/2025/06/How-to-Remember-Southern-Northern-and-Western-Blot-Tests-150x150.jpg)




Hi,
Any link to download – Books Recommended for Learning History Taking & Clinical Examination.
Thanks