In this article, we are going to share with you important points and high-yield Physiology notes for USMLE Step 1 & FCPS Part 1. One of the biggest hurdles faced by those preparing for USMLE Step 1 & FCPS Part 1 is the basic sciences. We have seen a lot of people struggle with basic medical science subjects especially Physiology, so we thought of writing a post and gathering high-yield Physiology Notes/Points for students who aspire to sit board or medical licensure exams i.e FCPS Part 1 or USMLE Step 1.
We hope you people find these High-Yield Physiology Notes/Points useful for your USMLE Step 1 & FCPS Part 1 Preparation! 🙂
GOOD LUCK! 🙂
CHECK ALSO:
High-Yield Anatomy Notes for FCPS Part 1
High-Yield General Pathology Notes for USMLE Step 1/FCPS Part 1
High-Yield Physiology Notes/Points for USMLE Step 1 & FCPS Part 1
Below are important points & high-yield Physiology notes for USMLE Step 1 and FCPS Part 1 exams.
We have also included a PDF document which contains important points & high-yield Physiology notes for FCPS Part 1 and USMLE Step 1. 🙂
SIZE: 1.7 MB
Hosted at: Google Drive
Download Link
RESPIRATION PHYSIOLOGY
- Between trachea and alveolar sac, the respiratory tract divides for 23 times. First 16 divisions are conducting zone up to terminal bronchioles. The rest are gas exchange zones
- Movement of diaphragm accounts for 75% change in intrathoracic volume during quite inspiration
- Most of the work of breathing(65%) is to overcome ELASTIC RECOIL (past MCQ). Other are airway resistance(28%) and viscous resistance (7%)
- In the upright position, the ventilation per unit volume is greater at the base of the lung than that of apex… the reason is intrapleural pressure is less negative at the base so alveoli are less expanded. At the apex, the intrapleural pressure is more negative and alveoli are more expanded i.e. the %age of max lung volume is greater. Because of the stiffness of the lung, the increase in lung volume per unit increase in the pressure is smaller when lung is initially more expanded so ventilation is consequently more at base
- Exercise is reported to increase the 2,3 DPG in 60 minutes… but n trained athletes this rise may not occur
- Four important functions of Hb. 1. Transport of O2. 2. Transport of CO2. 3. Buffer. 4. Transport of NO
- Chloride shift is mediated by a protein called BAND 3 one of the major membrane proteins.
- Of approximately 49ml of CO2 in dl of the ARTERIAL blood 2.6 ml is dissolved, 2,6 ml is carbamino compound and 43.8 ml is in bicarb form. In tissue 3.7 ml is added. O.4 ml stays in solution, o.8 ml forms carbamino compound and 2.5 ml forms bicarb
- Carotid and aortic bodies(GLOMUS) is made of TYPE I and TYPE II cells surrounded by fenestrated sinusoidal capillaries. Type I cells are called glomus cells which resemble chromaffin cells of adrenals and release catecholamines upon exposure to hypoxia and cyanide
BLOOD PHYSIOLOGY
- Total circulating blood is 8% of total body weight
- Active bone marrow forming the blood cells is called red marrow and inactive marrow is called yellow marrow. Inactive marrow is filled with fats.
- 75% bone marrow belongs to white blood cells producing myeloid series
- Neutrophils and monocytes are produced from a single precursor. There are se[arate pools for progenitors of megakaryocytes, lymphocytes, erythrocytes, eosinophils, and basophils
- Mast cells, Kupfer cells, dendritic cells, osteoclasts and Langerhans cells also originate from bone marrow
- Best source of hematopoietic stem cells is umbilical cord blood
- Average half life of neutrophils in circulation is 6 hours
- Nutrophils, eosinophils, and basophils are collectively called granulocytes/polymorphonuclear cells
- Eosinophils are abundant in GIT and respiratory mucosa
- Mast cells are abundant in areas rich in connective tissue eg beneath epithelium
- Monocyte leave the circulation and become macrophages in tissues. They do not reenter the circulation.
- Pluripotent uncommitted stem cells become committed by the action of IL1, IL6 followed by IL3(I,3,6 commits the stem cells, kind of love guru )
- Cytokines are hormone like molecules that act generally in paracrine fashion
- IL1 increases slow wave sleep and reduces appetite
- Platelets don’t have nuclei.They have half life of 4 days
- Splenectomy causes an increase in circulation platelets.
- Cytoplasm of platelets contains actin, myosin, glycogen, lysosomes, and two types of granules: a. Dense granules: they have nonprotein substances. They contain serotonin and ADP b. Alpha granules: contain clotting factors, PDGF
- Platelet production is controlled by colony stimulating factor and thrombopoietin. Thrombopoietin controls the maturation of megakaryocytes and is produced by kidney and liver.
- Osmotic fragility of RBC starts at 0.5% saline. Almost half the RBCs are lysed at 0.40 to 0.42% saline. Complete lysis occurs at 0.35% saline.
- 2.5 % hb in adults is HbA2
- Hb F has the ability to decrease the polymerization of deoxygenated HbS. Hydroxyurea causes HbF production and is used in treatment of HbS
- Blood group antigens are called aglutinogens
- Blood group antibodies are called agglutinins
- Blood group antigens are also present in salivery gland, saliva, kidney, pancrease, liver, lungs, testes, semen, and amniotic fluid
- A and B antigens are actually oligosaccharides that differ in their terminal suger. In RBCs they are mostly OLIGOSPHINGOLIPIDS and in other tissues they are glycoprotiens.(past MCQ)
- An antigen called H antigen is present in all RBCs in all individuals. In blood group A the A antigen is attached to H antigen, in blood group B the B antigen is attached to H antigen where as in blood group O no antign is attached to H antigen i.e terminal part of blood group O is H antigen(past MCQ). Blood group AB has both antigens at the terminal.
- Bilirubin rarely penetrates Blood brain barrier in adults. But in neonates and fetus the BBB is permeable to it an in erythroblastosis feotalis it causes KERNICTERUS
- If whole blood is allowed to clot and clot is removed, remaining is called serum. (plasma minus factor 2,5,8,fibrinogen is called serum)(past MCQ)
- Serum has high serotonin level due to breakdown of platelets.
- Thrombomodulin is produced by all endothelial cells except that of microcicculation of brain
- Thrombin is procoagulant in circulation blood. It becomes anticoagulant when it binds to thrombomodulin
- Lymph has lower protein content than plasma.
- Blood Storage
Storage of different blood products
- Whole blood is stored at 4° C for 3 weeks.
- Packed cells (RBCs) are stored at 1-6° C for 35 days.
- FFP (fresh frozen plasma) and cryoprecipitate can be stored at -40° C for 2 years.
- Platelets are stored at 22° C for 5 days
- mitral regurgitation =pansystolic murmur
- mitral stenosis =mid diastolic murmur
- aortic regurgitation =end diastolic murmur
- aortic stenosis =ejection Systolic murmur
- pulmonary regurgitation =diastolic murmur
- pulmonary stenosis =Systolic murmur
- throtoxicosis=innocent murmur
- decrease hematocrit =continuous murmur
- Gastric Motility increased by GASTRIN
- Gastric Motility decreased by CCK
- Intestinal Motility increased by CCK
- Intestinal Motility decreased by SECRETIN
- Gastric Emptying increased by Motilin
- Gastric Emptying decreased by CCK
- Gastric secretions inhibited by SECRETIN
- If Newborn to 14 years of age the most common cause is acute lymphoblastic leukemia
- If age is between 40 to 60 most likely cause will be AML and CML
- If age is more than 60 most likely causes r CLL and CML.
- Repeated blood Transfusion…..HAEMOCHROMATOSIS
- Multiple Transfusions….HYPOCALCEMIA
- Massive Transfusion. ….HYPERKALEMIA, HYPOCALCEMIA, and HYPOTHERMIA
- -Eosinophilia present in:
Hodgkin lymphoma and polyarteritisnodosa.
-PGI2__by endothelial cells
-TXA2__by platelets - Blood transfusion induced electrolyte balance is as follows:
-hypocalcemia
-hyperkalemia
-hypothermia
-metabolic acidosis
-left shift of oxy-hem curve
Hypokalemia and Hyperkalemia Important Points
|
Hypokalemia aggregates digoxin toxicity |
| Hypercalcemia cause pancreatitis & Pancreatitis causes hypocalcemia |
| Acidosis causes hyperkalemia & hyperkalemia causes metabolic acidosis |
| Hypokalemia causes alkalosis & Metabolic alkalosis causes hypokalemia |
| Hypokalemia inhibit insulin releases & Insulin causes hypokalemia |
| Insulin deficiency causes hyperkalemia & Hyperkalemia causes insulin release. |
| Hypokalemia causes rhabdomyolysis & Rhabdomyolysis causes hyperkalemia |
|
Sodium influx causes depolarization |
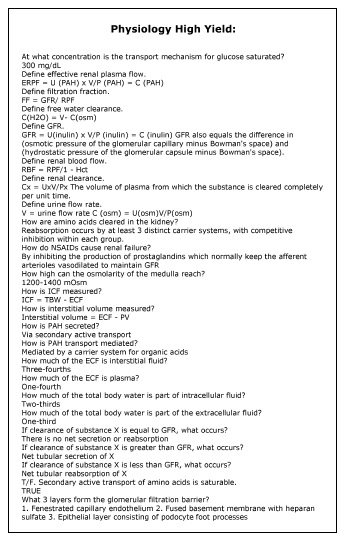
Renal Physiology
| 3 parts of fetal kidney and fate? | 1. Pronephros – degenerate @ week 4 2. Mesenephros – 1st trimester kidney then form male internal genitalia, ureteric bud extends into metenephros to form Collecting Duct, Renal Calyces, Renal Pelvis, Ureter. 3. Metenephros – permanent kidney – forms glomerulus through the distal tubule. |
| Which kidney is harvested for transplant and why? | 1. Left Kidney because it has a longer renal vein |
| How much of TBW is intracellular vs. extracellular? | 1. 1/3 is extracellular -> 25% is plasma volume -> 75% is interstitial volume 2. 2/3 is intracellular |
| What is the 60-40-20 rule? | 1. TBW = 60% of Total Body Weight 2. ICF = 40% of total body weight 3. ECF = 20% of total body weight |
| What is measured to determine plasma volume? | 1. Radiolabeled albumin – look at distribution |
| What is used to measure extracellular fluid volume? | 1. Inulin – can distribute to plasma compartment and interstitial volume but not into the cells |
| How do you calculate the intracellular fluid volume? | 1. Total body water – (ECFV via inulin) |
| What happens to GFR, RPF and the filtration fraction if blood plasma protein concentration increases? | 1. RPF does not change 2. GFR decreases 3. Filtration fraction decreases |
| What happens to RPF, GFR, and the filtration fraction if blood plasma protein concentration decreases? | 1. RPF no change 2. GFR increases 3. Filtration fraction increases |
| What happens if there is constriction of the ureter to RPF, GFR, FF? | 1. RPF NC 2. GFR decrease 3. FF decrease |
| How do you calculate reabsorption and secretion amounts for a given filtered substance? | 1. Filtered Load = GFR(Px) 2. Excreted Load = Ux(V) Reabsorbed = GFR(Px) – Ux(V) (if positive reabsorbed if negative then secreted). Secrete Load = (Ux)(V) – GFR(Px) |
| When does glycosuria begin? | 1. @ 160mg/dL, Na/Glucose cotransporters in the proximal tubule become saturated @ 350mg/dL (plateau of the reabsorption rate). |
| Why might there be glycosuria and aminoaciduria in pregnancy? | 1. Decreased reabsorption of glucose and amino acids at the level of the proximal tubule. |
| What 3 things increase renin secretion from the JGA? | 1. B1 receptor activation on the JGA 2. Decreased Na delivery to the MD in the distal convoluted tubule 3. Decreased BP sensed @ the JGA |
| Why does decreased Na delivery to MD cause an increase in renin secretion? | 1. Decreased Na delivery means more Na is being reabsorbed proximally in response to lower fluid volume, thus need to increase volume (renin secretion) |
| What are the 5 primary actions of ATII? | 1. ATI receptors in vasculature = vasoconstriction 2. Increased Aldosterone secretion 3. Increased Na/H exchanger activity in PCT to increase Na, HCO3, and H20 reabsorption 4. Increased ADH from posterior pituitary (supraoptic nucleus via neurophysins) 5. Increased thirst (hypothalamus) |
| Where is Angiotensin Converting Enzyme located? | 1. Lungs and Kidney –> Remember it is important for the degredation of bradykinin, inhibition can potentially lead to angioedema. |
| What does ADH primarily respond to?What does ADH primarily respond to? |
1. Decreases in osmolarity (remember this is sensed by the osmoregulator fenestrated areas in the brain) – At very low volume, ADH will be secreted |
| What does Aldosterone mostly respond to? | 1. Decreases in blood volume |
| How does ANP regulate volume? | 1. Leads to vasodilation via release of cGMP and then NO 2. Increases the GFR and increases Na excretion without increases in proximal tubule Na reabsorption. to net volume loss and Na loss –> This is why in hyperaldosteronism you will have normal fluid volume with hyponatremia, hypernatremia, and increased bicarbonate. |
| What substances/changes will shift potassium out of the cell? | DO Insulin LAbs: Digitalis HyperOsmolarity Insulin deficiency Lysis of Cells Acidosis Beta Antagonists (anti catabolic) |
| What substances/changes shift potassium into cells? (4) | 1. Insulin 2. Hypoosmarity 3. Alkalosis 4. Beta Adrenergic Agonists (increased Na/K ATPase) |
| What are the causes of anion gap metabolic acidosis? | MUD PILES CAT Methanol/Metformin Uremia DKA Propylene Glycol INH/Iron Lactic Acidosis Ethylene Glycol Salicylates (Late) Cyanide Alcohol/Acids Theophylline |
| What are the causes of normal anion gap metabolic acidosis? | HARD ASS Hyperalimentation Addison’s Disease Renal Tubular Acidosis Diarrhea Acetazolamide Spironolactone Saline Infusion |
| 1. What is Type 1 renal tubular acidosis? 2. What kidney stones is a person with type 1 RTA at risk for developing? |
1. Defect in collecting tubule’s ability to excrete H+ ions -> Resulting in hypokalemia, acidosis, 2. Increased risk of calcium phosphate kidney stones because increased pH or urine (>5.5) |
| 1. What is Type 2 renal tubular acidosis? 2. What is the effect on potassium levels and what disease state is it associated with? 3. What is urine pH? |
1. Defect in PCT ability to reabsorb HCO3- resulting in hypokalemia (at the distal collecting tubule/duct) 2. Fanconi’s Syndrome 3. Urine pH is <5.5 (Collecting duct and distal tubule can still secrete H+) |
| 1. What is Type 3 renal tubular acidosis? 2. What happens to urine pH in type 3 RTA? |
1. Hypoaldostronism – decreased collecting tubule response to aldosterone resulting in hyperkalemia 2. Urine pH will decrease because hyperkalemia messes up ammoniagenesis and thus NH3 buffering capacity |
Courtesy: Quizlet
Nerve Cell Physiology
| Describe the basic components of a nerve cell |
|
| Describe the nature of ionic permeability of the cell membrane | The lipid bilayer is impermeable to ions. Ion channels allow ions to cross the membrane. Ion pumps use energy to maintain the concentration gradients across the membrane. |
| Explain how the resting membrane potential is generated | Two forces work on ions: passive diffusion (moving down a concentration gradient) and electrostatic (repelling like forces). The electrostatic force generated by the separation of charged ions across the membrane prevents the complete diffusion of ions down their concentration gradients via ion channels. The net flow of ions across a cell membrane will be zero when the electrostatic and diffusion forces reach an equilibrium. The resting potential of a cell membrane is determined by the concentrations of ions present and their relative permeabilities across the membrane. |
| Explain how the action potential is generated | Applied current or excitatory input — voltage-gated Na+ channels open and Na+ rushes into cell — cell membrane is depolarized — Na+ channels begin to close as slower voltage-gated K+ channels open — cell membrane repolarizes and “undershoots” to cause an afterhyperpolarization — K+ channels close and membrane returns to resting potential |
| Explain the cause of the “refractory period” following action potential generation and discuss its functional significance | The Na+ channels have an inactive state following activation and cannot generate another action potential. Also, the opening of K+ channels hyperpolarizes the cell so that the membrane is unable to generate action potentials of equal strength. The refractory period limits how soon one action potential can be followed by another. |
| Explain how membrane potentials spread passively | In the absence of an action potential and voltage-gated Na+ channels, an injected current will travel passively down the axon. The magnitude of the current pulse decays exponentially, like a “leaky hose.” |
| Explain how action potentials propagate actively | Depolarization opens more Na+ channels farther down the axon, which causes further depolarization in a positive feedback cycle. |
| Explain why myelination allows for faster propagation of action potentials and how demyelination affects action potential conduction |
Myelination increases the membrane resistance, which prevents leakage of ions, makes the length constant of the axon longer, and current can spread farther before decay. Myelination decreases the membrane channels’ capacitance (the resistance to ion flow) , which decreases the time constant, and the membrane can depolarize faster. Demyelination increases the membrane capacitance, requiring more local current to depolarize for an action potential. The membrane resistance is lower, meaning a shorter length constant and limited spread of the local current. Action potentials are slowed or blocked in diseases of demyelination. |
Courtesy: Quizlet
HAPPY LEARNING! 🙂


![Best Books for FCPS Part 1 [Experience Based]](https://www.medicosrepublic.com/wp-content/uploads/2017/08/Best-Books-for-FCPS-Part-1-Experience-Based-218x150.jpg)
![High-Yield Pearls for FCPS Part 1 [Must Have]](https://www.medicosrepublic.com/wp-content/uploads/2017/08/High-Yield-Pearls-for-FCPS-Part-1-218x150.jpg)




![Gerstmann Syndrome Features Mnemonic [Easy-to-remember] Gerstmann Syndrome Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Gerstmann-Syndrome-Features-Mnemonic-150x150.jpg)
![Cerebellar Signs Mnemonic [Easy to remember] Cerebellar Signs Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Cerebellar-Signs-Mnemonic-150x150.jpg)
![Seizure Features Mnemonic [Easy-to-remember] Seizure Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Seizure-Features-Mnemonic-1-150x150.jpg)
![Recognizing end-of-life Mnemonic [Easy to remember]](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Recognizing-end-of-life-Mnemonic-150x150.jpg)

![Multi-System Atrophy Mnemonic [Easy-to-remember] Multi-System Atrophy Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Multi-System-Atrophy-Mnemonic-150x150.jpg)

![How to Remember Southern, Northern, and Western Blot Tests [Mnemonic] How to Remember Southern, Northern, and Western Blot Tests](https://www.medicosrepublic.com/wp-content/uploads/2025/06/How-to-Remember-Southern-Northern-and-Western-Blot-Tests-150x150.jpg)