Welcome to the golden topic — quite literally. ☀️
Neonatal jaundice is that classic yellow flag we all learn to chase early in paeds. And let’s be honest — you haven’t really done a paeds rotation until you’ve had a nervous parent ask, “Doctor sahab, yeh zard kyun ho gaya?”
Luckily, when you’ve been on-call with Dr. Bilal Chaudhary (our no-nonsense Paediatrician), you learn to categorize neonatal jaundice before your coffee even brews. ☕👶
🧠 Mnemonic for Causes of Neonatal Jaundice: “J.A.U.N.D.I.C.E”
| Letter | Cause | Explanation |
|---|---|---|
| J | Physiological Jaundice | Common, benign, appears after 24 hrs, peaks ~day 3. Baby’s liver’s just lazy. 😴 |
| A | ABO or Rh Incompatibility | Hemolysis due to maternal-fetal blood group mismatch. Think: anti-A/B or anti-D. |
| U | Urinary Tract Infection (UTI) | Less common but serious — especially if prolonged jaundice >2 weeks. 🚨 |
| N | Neonatal Hepatitis | Viral or idiopathic. Often with pale stools, dark urine. Rule out TORCH. 🦠 |
| D | Drugs (e.g., oxytocin, sulfonamides) | Some drugs in pregnancy can worsen jaundice by displacing bilirubin. 💊 |
| I | Infection (Sepsis) | Early-onset sepsis can present with jaundice — look for lethargy, poor feeding. |
| C | Cephalohematoma / Bruising | Extra RBCs broken down → extra bilirubin. That vacuum delivery has consequences. 🧠 |
| E | Enzyme Deficiency (G6PD, galactosemia) | Think hemolysis or metabolic error. Test if jaundice is early, severe, or prolonged. 🧪 |
🚼 Case from the Wards: A Neonate from Washuk, Balochistan
One morning, Dr. Bilal and I reviewed a 3-day-old baby from Washuk, brought in for “zard rang” (icterus) since day one. The child was irritable, febrile, and had poor feeding.
Initial thoughts? Physiological jaundice.
But bilirubin was >20 mg/dL on day 2.
A blood group mismatch? Nope.
We ran a sepsis screen — CRP was high. Culture grew E. coli.
Neonatal jaundice secondary to UTI — one of the more easily missed causes.
Started IV antibiotics — baby perked up in 48 hours. A good save. 😌
📚 Quick Tips for Clinical Exams (and Real Life)
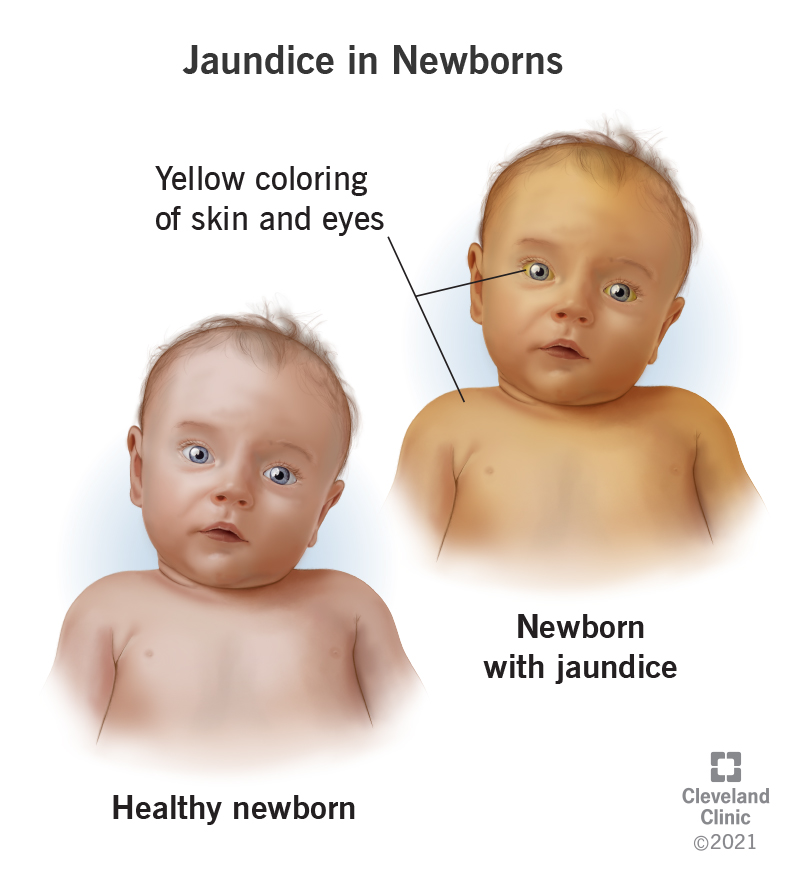
🔸 Pathological Jaundice red flags:
- Appears in <24 hours
- Bilirubin >5 mg/dL/day rise
- Direct (conjugated) bilirubin >2 mg/dL
- Persists >2 weeks
🔸 Conjugated hyperbilirubinemia = ALWAYS pathological!
🔸 Breast milk jaundice = peaks ~2nd week, benign, keep breastfeeding.
🔸 G6PD deficiency = suspect in males, especially if there’s a history of fava beans or naphthalene balls at home
I hope that you find this medical useful in your studies/clinical practice. Happy learning! 🙂
Authored by:
Dr. Aurangzaib Qambrani
MBBS | PLAB | MRCP-UK
General Medicine, Gastroenterology & CCU
Sheikh Khalifa Bin Zayed Hospital, Quetta 🏥

![How to Remember Southern, Northern, and Western Blot Tests [Mnemonic] How to Remember Southern, Northern, and Western Blot Tests](https://www.medicosrepublic.com/wp-content/uploads/2025/06/How-to-Remember-Southern-Northern-and-Western-Blot-Tests-218x150.jpg)






![Gerstmann Syndrome Features Mnemonic [Easy-to-remember] Gerstmann Syndrome Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Gerstmann-Syndrome-Features-Mnemonic-150x150.jpg)
![Cerebellar Signs Mnemonic [Easy to remember] Cerebellar Signs Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Cerebellar-Signs-Mnemonic-150x150.jpg)
![Seizure Features Mnemonic [Easy-to-remember] Seizure Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Seizure-Features-Mnemonic-1-150x150.jpg)
![Recognizing end-of-life Mnemonic [Easy to remember]](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Recognizing-end-of-life-Mnemonic-150x150.jpg)

![Multi-System Atrophy Mnemonic [Easy-to-remember] Multi-System Atrophy Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Multi-System-Atrophy-Mnemonic-150x150.jpg)

![How to Remember Southern, Northern, and Western Blot Tests [Mnemonic] How to Remember Southern, Northern, and Western Blot Tests](https://www.medicosrepublic.com/wp-content/uploads/2025/06/How-to-Remember-Southern-Northern-and-Western-Blot-Tests-150x150.jpg)