There’s a special kind of terror that hits parents at 2 a.m. — a loud, barking cough followed by a frantic sprint to the ER. The child sounds like a seal with laryngitis, and the mother looks like she’s aged five years in five minutes.
That’s when Dr. Bilal Chaudhary, our resident pediatric legend, calmly says,
“It’s just croup. We’ll nebulize and hydrate. No need for a CT or a cardiology referral this time, Dr. Imran.” 😅
So today, let’s decode Croup — and help you remember its classic symptoms with a mnemonic even a sleep-deprived MO on night duty won’t forget:
Croup Symptoms Mnemonic: “BARKS”
| Letter | Symptom | Clinical Nugget |
|---|---|---|
| B | Barking Cough | Harsh, seal-like. The kind you hear through two closed doors and a panic-stricken parent. |
| A | Afebrile (or Mild Fever) | Usually viral. High fever? Think epiglottitis or bacterial tracheitis instead. |
| R | Respiratory Distress | Inspiratory stridor, nasal flaring, intercostal retractions = classic picture. |
| K | Kiddos (Age 6 mo – 3 yrs) | Peak incidence: toddlers. If a 10-year-old has it, question the diagnosis 🤨 |
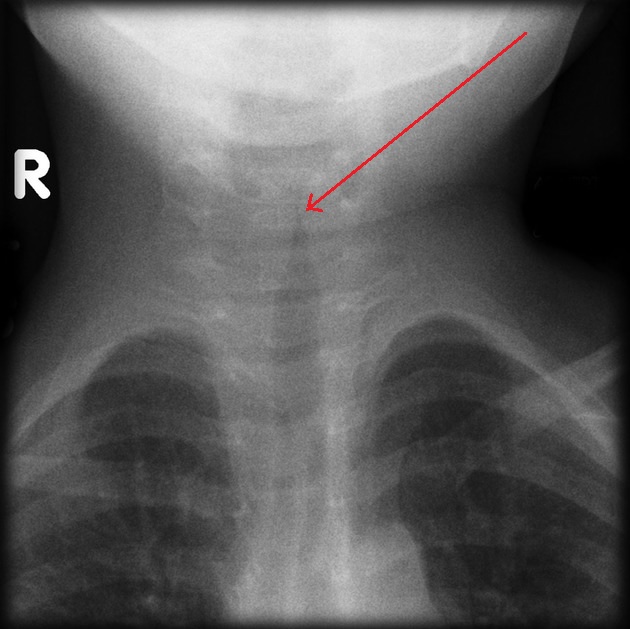
| S |
Stridor (Inspiratory) Steeple sign (X-ray) |
Worsens at night. Doesn’t need a bronchoscopy at 3 a.m., trust me. |
👶 Croup in the Cold Nights of Kohlu, Balochistan
A young mother brought her 18-month-old from Kohlu, bundled in four shawls and clearly distressed.
“Doctor sahab, he’s barking like a dog at night.”
She wasn’t exaggerating.
Classic “B.A.R.K.S” — barking cough, inspiratory stridor, mild fever.
Dr. Bilal Chaudhary calmly gave nebulized epinephrine and a dose of dexamethasone, and within an hour, peace was restored — except for the ward boy, who kept asking if we should admit him to CCU (thanks, internal referrals).
🤓 Quick Exam Tip (because MRCP and ward rounds are both brutal)
Barking cough + stridor + child under 3 = Croup.
Management = Dexamethasone ± Nebulized Epinephrine.
Don’t forget to reassess after 2 hours post-nebulization.
And yes, admit if: persistent stridor at rest, poor feeding, or oxygen requirement.
💬 From the Wards at Sheikh Khalifa
One of my most mildly traumatic calls was when Dr. Danish Ramzan rang me at 1:45 a.m., convinced his nephew had a tracheal obstruction.
Turned out to be textbook croup.
I prescribed dexamethasone and warm tea (for the parents). He still owes me biryani for that night.
I hope that you find this medical useful in your studies/clinical practice. Happy learning! 🙂
Authored by:
Dr. Aurangzaib Qambrani
MBBS | PLAB | MRCP-UK
General Medicine, Gastroenterology & CCU
Sheikh Khalifa Bin Zayed Hospital, Quetta 🏥

![How to Remember Southern, Northern, and Western Blot Tests [Mnemonic] How to Remember Southern, Northern, and Western Blot Tests](https://www.medicosrepublic.com/wp-content/uploads/2025/06/How-to-Remember-Southern-Northern-and-Western-Blot-Tests-218x150.jpg)






![Gerstmann Syndrome Features Mnemonic [Easy-to-remember] Gerstmann Syndrome Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Gerstmann-Syndrome-Features-Mnemonic-150x150.jpg)
![Cerebellar Signs Mnemonic [Easy to remember] Cerebellar Signs Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Cerebellar-Signs-Mnemonic-150x150.jpg)
![Seizure Features Mnemonic [Easy-to-remember] Seizure Features Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Seizure-Features-Mnemonic-1-150x150.jpg)
![Recognizing end-of-life Mnemonic [Easy to remember]](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Recognizing-end-of-life-Mnemonic-150x150.jpg)

![Multi-System Atrophy Mnemonic [Easy-to-remember] Multi-System Atrophy Mnemonic](https://www.medicosrepublic.com/wp-content/uploads/2025/06/Multi-System-Atrophy-Mnemonic-150x150.jpg)

![How to Remember Southern, Northern, and Western Blot Tests [Mnemonic] How to Remember Southern, Northern, and Western Blot Tests](https://www.medicosrepublic.com/wp-content/uploads/2025/06/How-to-Remember-Southern-Northern-and-Western-Blot-Tests-150x150.jpg)